Bilateral Oophorectomy and Salpingectomy: Understanding the Procedures
The world of women's health can often be complex and overwhelming, particularly when it comes to surgical procedures. Among the various options available, bilateral oophorectomy and salpingectomy have significant importance, especially for those facing specific health challenges. This article aims to provide a comprehensive overview of these surgical interventions, shedding light on their indications, procedures, risks, and benefits, enhancing your understanding while supporting your health journey.
What is Bilateral Oophorectomy?
A bilateral oophorectomy is a surgical procedure that involves the removal of both ovaries. This procedure can be performed laparoscopically (minimally invasive) or through a larger open incision. While the decision to undergo this procedure can be daunting, it is often necessary for a variety of medical reasons.
Indications for Bilateral Oophorectomy
- Ovarian Cancer: One of the primary reasons for this surgery is the presence of malignant growths in the ovaries.
- Endometriosis: For women suffering from severe endometriosis, this procedure may alleviate chronic pain and other associated symptoms.
- Genetic Predisposition: Women with BRCA1 or BRCA2 gene mutations may choose this surgery to reduce their risk of developing breast and ovarian cancers.
- Benign Ovarian Tumors: Non-cancerous tumors may also necessitate oophorectomy if they cause significant discomfort or complications.
What is Salpingectomy?
A salpingectomy is the surgical removal of one or both fallopian tubes. This procedure can be performed alongside a bilateral oophorectomy or as a standalone treatment. Salpingectomy is increasingly recognized in the context of preventive surgery for hysterectomy patients or those with certain risk factors for ovarian cancer.
Indications for Salpingectomy
- Ectopic Pregnancy: A common reason for performing a salpingectomy is to address an ectopic pregnancy, where the fertilized egg implants outside the uterus.
- Pelvic Inflammatory Disease (PID): PID can cause damage to the fallopian tubes, necessitating their removal to prevent recurrent infections.
- Risk Reduction for Ovarian Cancer: Women at high risk for ovarian cancer may opt for salpingectomy to reduce their risk while preserving their ovaries.
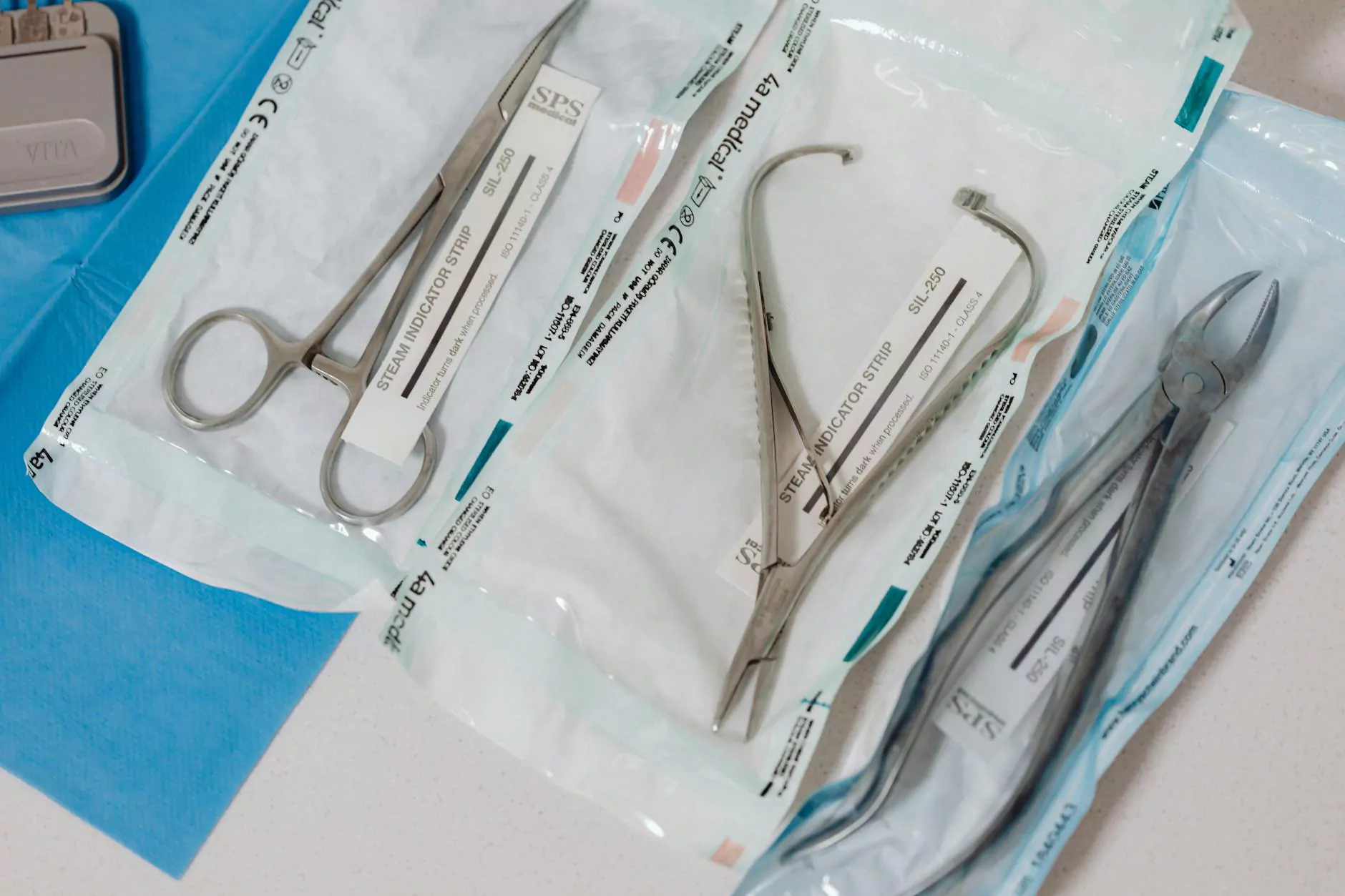
The Surgical Procedures Explained
Understanding the procedures of bilateral oophorectomy and salpingectomy can help decrease anxiety associated with surgery. Here’s a detailed look at what to expect during each procedure:
Bilateral Oophorectomy Procedure
The surgical approach may vary based on the patient's condition:
- Pre-operative Assessment: Before surgery, a thorough evaluation will be conducted, including medical history, physical exams, and imaging studies.
- Anesthesia: Patients are generally given general anesthesia to ensure they are unconscious and pain-free during the operation.
- Accessing the Ovaries: Surgeons may use laparoscopic techniques, which involve small incisions and the use of a camera for guidance. In cases requiring exploration, a larger incision may be necessary.
- Ovary Removal: The ovaries are carefully dissected from their surrounding tissues and removed.
- Closing the Incisions: Once the surgery is complete, the incisions are closed with sutures or staples.
Salpingectomy Procedure
The salpingectomy procedure shares similarities with the oophorectomy:
- Assessment and Anesthesia: Like oophorectomy, patients undergo evaluations before receiving general anesthesia.
- Incision: The surgical team will determine the best approach (laparoscopic or open surgery) based on individual circumstances.
- Removal of the Tubes: The fallopian tubes are carefully excised from the uterus and ovaries, ensuring no damage to nearby structures.
- Wound Closure: The final step involves closing the incisions, followed by a recovery period in the hospital.
Benefits of Bilateral Oophorectomy and Salpingectomy
Both surgical procedures offer myriad benefits, particularly for women at risk or suffering from specific conditions. Here are some key advantages:
Physical Health Benefits
- Cancer Risk Reduction: Removing ovaries and fallopian tubes decreases the risk of developing ovarian cancer significantly.
- Pain Relief: For conditions like endometriosis, these procedures may substantially decrease pelvic pain and discomfort.
- Elimination of Hormonal Imbalances: In cases of severe hormonal disorders, the removal can stabilize hormone levels, improving quality of life.
Psychological Benefits
Making the decision to proceed with bilateral oophorectomy and salpingectomy can also lead to psychological benefits:
- Peace of Mind: Knowing that the risk of certain cancers has been mitigated can alleviate anxiety that many women face.
- Improved Quality of Life: Reduction or elimination of pain and symptoms can restore normalcy and enhance life satisfaction.
Potential Risks and Considerations
While both procedures are valuable tools in women's health, it is crucial to recognize their potential risks:
Common Risks
- Infection: As with any surgery, there is a risk of infection at the incision site or internally.
- Bleeding: Hemorrhaging during surgery can occur, necessitating blood transfusions or additional interventions.
- Damage to Surrounding Organs: There is a risk that nearby organs, such as the bladder or intestines, may be inadvertently injured during surgery.
Long-term Considerations
After a bilateral oophorectomy, women enter menopause because both ovaries are removed. It’s essential to discuss:
- Hormone Replacement Therapy (HRT): HRT can help manage menopausal symptoms and reduce risks associated with hormonal deprivation.
- Emotional Support: Psychological adjustments are vital, and women should consider counseling or support groups to cope with the changes.
Recovery Process
Understanding what to expect after surgery can help smooth the recovery process:
Immediate Recovery
- Hospital Stay: Patients may require a night or two in the hospital for monitoring.
- Pain Management: Pain relief medications will be provided to ease discomfort.
At-Home Recovery
Once discharged, it is crucial to follow post-operative instructions carefully:
- Activity Restrictions: Patients should avoid strenuous activities and heavy lifting for several weeks.
- Follow-Up Appointments: Regular check-ups with the healthcare provider are essential to monitor healing and address any concerns.
- Diet and Hydration: Maintaining a well-balanced diet and staying hydrated are vital during recovery.
Conclusion
In conclusion, understanding bilateral oophorectomy and salpingectomy is integral for women facing health challenges related to their reproductive systems. This knowledge empowers patients to make informed choices regarding their health, alleviating anxieties and improving outcomes. We encourage you to discuss any concerns with your healthcare provider. For patients seeking specialized care, clinics like drseckin.com provide expert services in the fields of gynecology and women's health, helping you navigate your health journey with confidence and care.
Stay informed and prioritize your health by reaching out for assistance and guidance when needed.